On a breezy summer’s morning in December 2014, 25-year-old Jess Pereira woke to find that her lower back felt stiff and sore. Jess was an active young woman, her mind focused on the European holiday she was planning with her husband, Andrew, and as she eased herself out of bed, she surmised it was nothing more than the legacy of some intensive gym sessions.
The pain, however, didn’t go away.
A few weeks later, by which time it was also shooting down her leg, she saw her GP. After an MRI scan, the doctor delivered the chilling words: “You have tumours that could be cancer.”
More tests confirmed the worse.
Jess had cancer: a rare, aggressive form of lymphoma to be precise.
“I didn’t break down and sob until I told my husband and family over the phone,” recalls Jess. “At 25, I was staring death in the face.”
“I didn’t break down and sob until I told my husband and family over the phone”
Jess Pereira
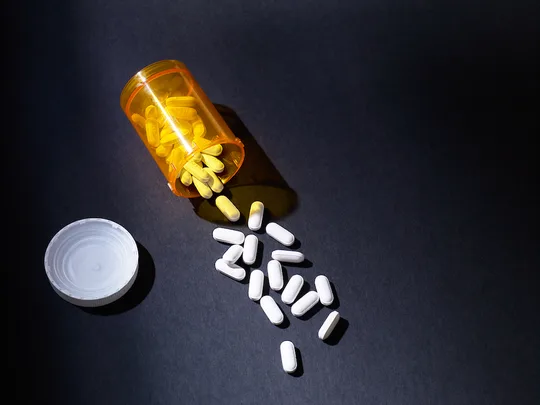
What followed were months of “sheer hell” as Jess faced excruciating pain, radiation therapy, lumbar punctures every 10 days and chemotherapy.
To cap it of, her enforced absence meant she lost her new job as a legal secretary at a top Sydney firm.
Three times her cancer appeared to be responding to treatment only to return, with tumours appearing in her hip, neck, chest, abdomen, arms and legs. In June 2015, her specialist said she thought they had run out of options. “I remember thinking that I wasn’t going to make it to my 26th birthday,” says Jess. “But then my specialist contacted me and said she’d done some research and found a newer drug called Crizotinib.”
The only catch? It would cost $7400 a month and Jess needed it for at least six months of treatment. “I felt completely overwhelmed – how would I ever raise that kind of money? I’m quite shy and the prospect of calling on others for money made me feel like a charity case.”
Family and friends rallied and raised $23,000, holding morning teas in their workplaces and passing the hat around at clubs; one friend even sold scarves and beanies online. It meant Jess was able to start treatment with the drug in June 2015.
“The improvement was incredible,” she recalls. “Within two weeks, the searing pain and joint stiffness began improving. A month after starting the drug, I had a PET scan and there were no tumours in my body. I can’t tell you how incredibly uplifting that was.”
The charity Rare Cancers Australia then started crowdfunding to raise funds for Jess to continue treatment.
“But that money [will] run out in December and I am terrifed that I might have to stop treatment, and maybe I will die,” she says, softly.
And here is the cruel paradox. The luck of the draw, if you can call it that. Had Jess’s cancer started in her lungs and not her back, she would have been able to get the very same drug for just $37.70 per month. The difference? The government subsidises the drug for some forms of cancer, but not others.
In Australia, when a drug is listed on the Pharmaceutical Benefts Scheme (PBS), the government subsidises the cost by paying the pharmaceutical company a negotiated price, which means the patient has to pay far less. But frst a cancer drug has to get on to the PBS, and critics say there are a number of issues with this system. For one, they argue that the approval process moves at a glacial pace and is costing patients their lives; they also want to see the system streamlined.
Secondly, they say drugs on the PBS should be approved for the treatment of a wider range of cancers.
Until progress is made, doctors are left facing an ethical dilemma. Specialists question whether to tell patients, who are losing their hair and suffering pain, nausea and extreme fatigue, that there are drugs that might help, but they can cost nearly $8000 every month.
“Forty-one per cent of oncologists said they were less likely to mention a cancer drug if it was not subsidised, because the knowledge that the patient could not afford it would be too distressing for [them],” says Professor John Zalcberg, co-chair of Cancer Drugs Alliance and head of the Cancer Research Program at Monash University.
Those patients confronted with the sky-high price tags (set by pharmaceutical companies) of drugs not on the PBS are faced with a terrible choice: go without the drug that may extend their life, or make desperate attempts – such as selling the house – to raise the money.
Like Jess, Anita, a 45-year-old accountant from Brisbane and mother of two boys, aged 7 and 11, was stunned when she was diagnosed with cancer after suffering from a persistent cough for two years.
“I was a fit and healthy non-smoker, yet suddenly a specialist was telling me I had an inoperable, rare lung cancer and the survival rate was only 10 per cent,” she says. “I lay awake at night worrying for my husband, and felt heartbroken that I would not live long enough to see my two boys even start high school.”
After radiation and several rounds of chemo – which caused lethargy, nausea and hair loss – did little to slow Anita’s cancer, Crizotinib was her only option.
“I lay awake at night worrying for my husband, and felt heartbroken I wouldn’t live to see my two boys start high school.”
Anita
While Crizotinib is often an improvement on chemotherapy and may extend life for patients, it is not a lifesaver or a miracle drug. A study in the New England Journal Of Medicine found that the probability of one-year survival was 84 per cent with Crizotinib and 79 per cent with chemotherapy.*
But, for some people like Anita, the chemotherapy simply does not work.
She found Critzotinib far more tolerable and effective than her chemo. “It has been fantastic,” she explains. “After 13 months of treatment my tumour has halved in size. The drug also has far fewer side effects, so I feel and look well, which has helped my boys to better cope with handling my disease – as the more sick I look the more upset they are.”
Anita, like Jess, was initially forced to raise funds to pay for treatment with Crizotinib – at that point, the drug was not on the PBS, even though it had already been approved in more than 65 countries. Anita’s parents paid for the frst month and, with friends, helped pull together $20,000 using Facebook and fundraising. Crowdfunding initiatives through Rare Cancers Australia raised another $4000.
Then, on July 1 2015, Crizotinib was added to the PBS. For Anita, this meant only paying $37.70 a month for her lifesaving treatment. “I was so relieved that I sobbed and sobbed and we had a big celebration,” recalls Anita. “It meant I could step of that exhausting merry-ground of doing TV and newspaper interviews to raise money for my treatment. It was like an enormous weight had been lifted from my shoulders.”
But Anita still faces obstacles. Her cancer will eventually outsmart the medication. “For that reason, the drug company has developed three new generations of this drug, which are available in America but not here in Australia,” explains Anita. “I live in fear that the next generation of these drugs may fall through the PBS black hole and not be approved by the time I need them; this will cut my life short. That possibility hangs over my life like a big, dark cloud.”
So what’s the hold-up? And why is our system favouring some patients over others? Blame it on our ineffcient and outdated PBS, say its critics. Australia is one of the slowest countries in the Organisation for Economic Co-operation and Development (OECD) in terms of approving cancer medicines for use and for government subsidy, according to a Deloitte report funded by a taskforce made up of many of the world’s biggest pharmaceutical companies.ˆ It found that some drugs that were listed in countries like the UK, France and Germany were not listed in Australia until six or seven years later.
These statistics are even worse for the 44,000 Australians each year who are diagnosed with a rare or less common cancer. The drugs that could help them are less studied by drug companies, less trialled, and therefore less likely to gain approval. As Jess experienced, just because a drug is on the PBS does not mean it’s available to patients with all forms of cancer. Rather it is only approved for specific permutations of the disease.
“The current system fails to take into account that treatments are becoming more targeted … that cancers in diferent parts of the body often have similar causes,” says Professor Zalcberg. “Instead, our PBS approves drugs according to [the cancer’s] location in the body and fails to acknowledge the causal mechanisms that make cancer similar.”
The job of approving PBS drugs falls to the Pharmaceutical Benefts Advisory Committee (PBAC), which meets three times a year. This in itself is an issue, say specialists. “Waiting to access new treatment for months or even a year can mean the difference between life and death,” says Professor Zalcberg. The issue has raised such concern that in 2014, a cross-party Senate committee was formed. Their report, released in September 2015, outlined the “grim reality”, stating that “delays in access to new and innovative cancer medicines can be measured in loss of quality of life and years and lives lost”.
“Families are being forced to sell their homes, and use up savings and superannuation at a time when they are already suffering maximum stress from the anxiety, upset and upheaval of living with cancer,” says Richard Vines, co-founder and chair of Rare Cancers Australia*, whose Sick or Treat crowdfunding program – which helps people with rare cancers pay for their treatment – has raised almost one million dollars since it began in October 2014.
Families are being forced to sell their homes”
Richard Vines, Rare Cancers Australia
In this debate, however, it’s impossible to ignore the issue of the bottom line. The PBAC say that the public purse can’t aford to put every new cancer drug on the PBS or it would blow out our health budget; many experts also believe that the pharmaceutical companies should shoulder some of the responsibility by lowering the cost of these drugs.
As it stands, in the 2013–14 financial year, the PBS cost the government $9.6 billion, a 1.1 per cent increase on the previous year. Going forward, the government will consider the Senate report’s recommendations, says Minister for Health Sussan Ley, including a more streamlined and flexible approach.
More broadly, is it fair to devote so many tax dollars to the scheme, dollars that could be used elsewhere in health to potentially benefit more people? These are the harsh realities beyond the heart-wrenching personal stories.
No-one knows better than Dannii Raisher, 32, from Victoria, that this issue can be a matter of life and death. In March 2015, her husband and childhood sweetheart, Shane, died from the melanoma he had been diagnosed with at 18. Three months later, Keytruda, the drug that might have kept him alive, was approved to be listed on the PBS.
“Simply trialling the drug for three months had reduced his tumour size by 70 per cent and kept the cancer at bay for 12 months after he stopped taking [it],” says Dannii. “But we couldn’t continue to find the $10,500 every three weeks to pay for the treatment.”
Instead they lobbied the federal government. Their petition on Change. org attracted 170,000 signatures and was instrumental in getting the drug approved. But it was all too late for Shane, who died at 32, leaving behind his son Jett, not quite three, and Dannii, who was 21-weeks pregnant with their second son.
“Once [the drug] was finally put on the PBS in June 2015, it was still not available until September – six months after Shane’s death,” she remembers. “Giving birth only months after [he] died was incredibly emotional … It is heartbreaking that Shane never got to hold his newborn.
Meanwhile, Jett keeps waiting for his daddy to come home. That’s what the bean counters don’t see – how this ineffcient and inequitable system with all its red tape robs families like ours of precious time together.
“Shane was a fighter and a very positive person. But he was incredibly angry and disappointed with a system where access to some cancer treatments is determined by how rich you are.”
Jess Pereira agrees. If she can’t find more money soon she will have to stop the treatment that is helping to keep her alive. In the meantime, she’ll keep fighting, starting with posting a new petition at change.org/ rare cancers. “Cancer doesn’t discriminate,” she says. “So the government shouldn’t discriminate either.”
To donate to Jess Pereira’s drug treatment, click here
 Getty
Getty