I was always aware of ovarian cancer but didn’t know much about it prior to my diagnosis at 22. Growing up, I remember hearing about breast cancer or skin cancer, but never ovarian. It’s hard to escape the idea of cancer—every second news report talks about it. I was always scared it could happen to me. But with no family history of cancer, I felt like my concerns were more of an anxiety than a real fear.
Like most ovarian cancer symptoms, my initial ones were very vague and could easily be dismissed. I had this on-and-off pain in the side of my stomach that began in the first week of August. I’m lactose and fructose intolerant, so I shrugged it off as being related to that. I always had mild stomach pains. It wasn’t until I complained about the pain to my mum and sister five days later, with them both suggesting I speak to a GP, that I took the pains seriously—I was pointing to a spot near my ovaries.
You should always listen to your body—after five days, I knew the pain in my side wasn’t ‘normal’ for me. Women need to know and understand their bodies, so when abnormalities arise, we can go seek assistance. If someone is worried about anything, it’s always safer to go to a GP and get it checked out.
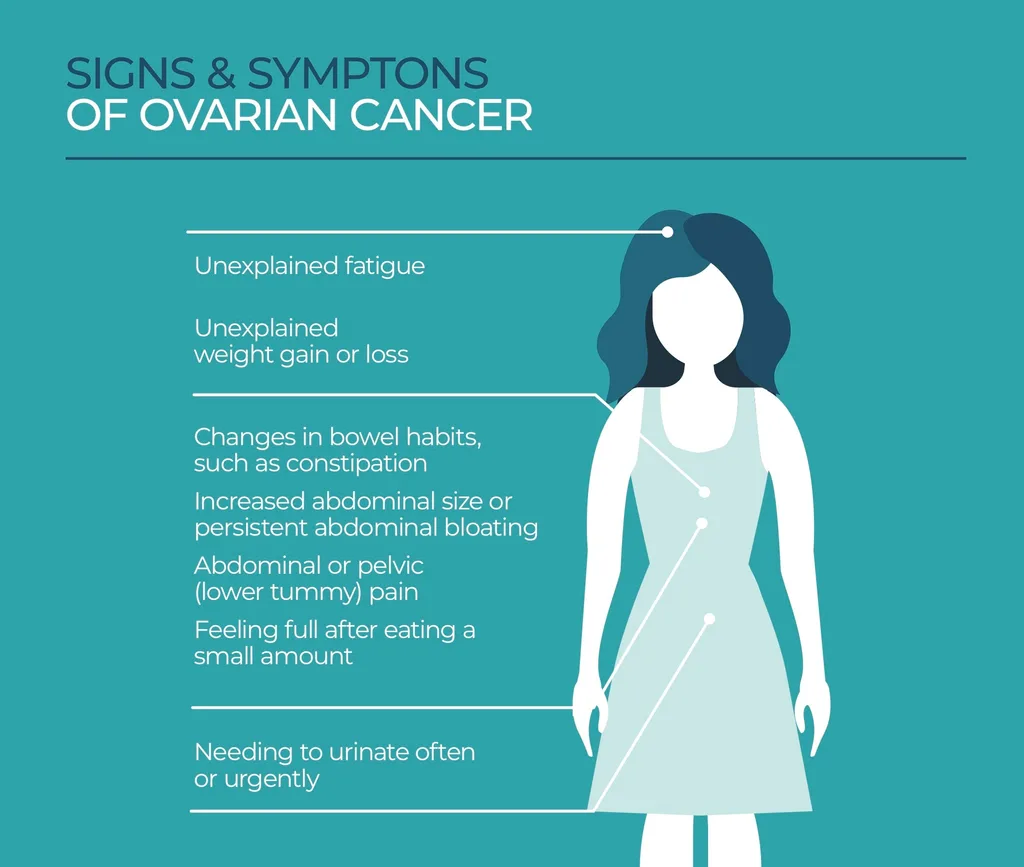
Unfortunately, ovarian cancer symptoms are so vague that it is hard to discern—especially as there are currently no early detection tests.
My whole situation? Just luck. My normal GP was actually on maternity leave and when I called to speak to someone at my local GP’s office, it was almost closing time and only one other GP had an availability to call me via Telehealth. I had never met this GP, but she told me to come into the clinic so she could have a look.
She was new to the clinic and referred me for an ultrasound the next day. While I’ve had a different GP from the same clinic to take care of me throughout my cancer journey, I did reach out to the GP who I first spoke to, who revealed she has a background of working with ovarian cancer and with my gynaecological oncologist. I’m just very thankful and blessed that she never dismissed what I thought was a simple pain in my side.
The possibility of this pain being related to cancer frightened me. In the media, cancer is always linked to death, baldness, losing lots of weight due to not being able to eat and being stuck in a hospital. All of these stereotypes scared me. Only a day after I saw my GP and a few hours after getting an ultrasound did the word ‘cancer’ start to get thrown around. I didn’t believe it at first. I was definitely in denial and didn’t want it to be true.
I had an ultrasound on Wednesday morning. Following the appointment, I logged straight onto an online university class. Then I was called by a different GP explaining that the ultrasound was showing cancerous tumours around my ovaries. Because it was near the end of the day, she was unable to book any appointments with a gynaecologist. She explained that my best option was to go to an emergency department the next day, as they would be able to get all testing done nice and quick.
The next morning I went to emergency with my mum and waited for around four hours to actually be seen, even attending a virtual online workshop whilst in the waiting room. My mum was prohibited from going up to the short-stay unit with me. This was terrifying, I couldn’t imagine not having my mum by my side the whole time. But that’s the issue with being diagnosed during Melbourne’s Stage Four Lockdown. While there, I met a gynaecologist, had another ultrasound, then a COVID-19 test, blood test and CT scan.
The whole experience was quite traumatic for me, as I was continuously told that I most likely have cancer and I would probably have to undergo chemotherapy. They debated keeping me overnight, but I just couldn’t stop crying, so my mum came to pick me up at two am the next morning. On Friday and I received a call from the secretary of my gynaecological oncologist—my surgeon—that was referred by the gynaecologist in the emergency department, informing me that they would be booking in surgery for the upcoming Monday.
The day was just a blur. I’d hardly slept since I’d come home so late from the emergency department and I had various phone calls from my GP, the gynaecologist from emergency department, and now the new surgeon. Waiting a whole weekend for the surgery was agonising but I tried to keep myself distracted and calm. At this point, only four close friends in my life knew and a small number of family friends. Everyone was just in shock and disbelief. Monday morning arrived and my mum, dad and sister dropped me off at the door of the hospital and I had to go alone to get admitted.
Ovarian cancer can only be diagnosed through surgery. Due to the size of my tumours, I had to have a full laparotomy. Meaning, they had to cut from my belly button to below my bikini line. My surgeon was also debulking, physically cutting out any tumours she could, while simultaneously taking as many samples as possible of tissue to be biopsied. The biopsy results took 5 days.
On the fifth and final night of being in hospital after surgery—only six days after I saw the GP—I found out I had Stage Three ovarian cancer.
My surgeon came to my hospital room and I put my family on loudspeaker to hear the results. It’s still quite traumatic to recall that conversation. I instantly feared that I was dying. I was horrified about the thought of chemo and especially what would happen to my hair.

I have always had long hair. I know it can sound very superficial, but keeping my hair made me feel ‘less’ sick. I never wanted to ‘look’ like I had cancer. That’s when my surgeon told me about cold-capping and the possibility of saving my hair. I couldn’t stop crying during and after that conversation. It’s taken a long time for me to fully feel comfortable about recalling that whole experience and to even admit to myself that I have cancer.
It took at least eight to ten weeks for me to recover from that surgery, as I had to relearn how to walk and stand up with a physio. I was in immense pain when just laughing or sneezing. Prior to the surgery, they suspected I had ovarian cancer, but they couldn’t be sure until the biopsy report came back. Another reason why we need to have more funding for early detection. Surely, we need a new way to diagnose women without having to do such an intense surgery? Luckily, during a second surgery on New Year’s Eve I had only a small laparoscopy (keyhole), which only required three small cuts on my stomach, and I was allowed to go home the next day.
I had begun my Master of Management (Human Resources) in the first week of August. It was only during my second class of the course that I first experienced the pain in the side of my stomach. I had worked so hard to get into this graduate course, I was determined to continue. Deferring wasn’t an option I wanted to take. As soon as I found out the extent of my condition, I emailed all my lecturers to discuss my possibilities.
I had amazing support from one of my lecturers. He made it clear that he wanted me to succeed in the subject and that he was willing to work with me to ensure that I would be able to achieve my goal of completing the subject whilst going through my medical treatments. Ultimately, I had the exam for this subject in between chemo rounds and my final mark exceeded my expectations.
For me, studying was the best distraction from my health battle, and I don’t know how I would have coped had I not continued with it.

I wanted everything to be as normal as possible with my friends during treatment. I remember asking a friend how she was, but she was more concerned about me. I insisted that we talk about her problems—I wanted her to feel comfortable to speak freely with me. Unfortunately, I found that some friends didn’t know what to say, even to this day. It has created a strain in many friendships. It’s a sad reality that many people going through a cancer do experience.
It’s astonishing to see how few people ask, ‘are you okay?’ when you’re going through cancer treatment. For me, it was quite an isolating and sad period of my life to see how many people who I thought were really close to me never reached out. But there were some friends who really did rise up to the challenge and I’m forever thankful for the support I received from them.
In terms of my family, they have been my rock. They have helped me through this whole process, and I can’t imagine doing it without them. My sister and parents always insisted that we need to find the humour in this situation and not sit in a pity party. It helped us get through the difficult moments. My mum had to take on a huge responsibility, becoming my full-time nurse by injecting me with anti-clotting injections every day after surgery, washing my hair and sitting with me during chemo treatments. Despite me being the one with ovarian cancer, my whole family have suffered with me.
Having ovarian cancer, especially at a young age, meant it was difficult to find the right support. It’s not commonly experienced amongst young women and it was hard to find someone who was going through the same thing. My GP has been amazing and called me fortnightly to check up on my progress and to see if I needed anything. It was Ovarian Cancer Australia who provided me with an ovarian cancer nurse who was able to talk through all my concerns and fears with me, and provide me with specialist advice. OCA also provided my mum with a counsellor which was extremely helpful.
I wish people would understand that ovarian cancer is one of the most poorly funded cancers in Australia. There has been little improvement in the way of medical advances and treatments used to battle this disease – despite it having the highest mortality rate amongst gynaecological cancers.
I also believe that gynaecological cancers are less commonly discussed due to the stigma associated with this part of the female body. We need to be able to initiate these difficult conversations so that these discussions on how to detect and prevent these types of cancers can be had.
Ovarian cancer is the deadliest gynaecological disease. Every year, more than 1600 Australian women are diagnosed with the disease and it claims the lives of more than 1000. Help raise awareness of the dangers of ovarian cancer. Share Chloe’s story and donate to Ovarian Cancer Australia here. Ovarian Cancer Australia is also tripling every dollar donated throughout February to help assist researchers, who believe they’ve never been closer to a cure.










